Atlas of Nonsexually Transmitted Genital Conditions. Fixed Drug Eruption, Psoriasis, Penile Fracture, Penile Sclerosing Lymphangitis, Anal Fissure, Perianal Fistula, Behçet Syndrome, Genital Pyoderma, Erythrasma, Tinea Cruris, Vitiligo, Lichen Simplex Chronicus, Contact Dermatitis, Lichen Planus, Fordyce Spots, Pearly Penile Papules and Tyson Glands,
OVERVIEW
Many dermatologic conditions can affect the genitals, and some anatomic variants, both genital and nongenital, may be mistaken for abnormal conditions by patients or their health care providers. Not surprisingly, sexually active persons with genital symptoms often present to providers with concerns about STD. Entire textbooks have been written on the topic of genital dermatology, and it is beyond the scope of this book to provide a comprehensive overview. Examples of a few conditions are presented, with emphasis on those that are likely to affect younger persons or are easily confused with STDs.
Fixed Drug Eruption
Fixed drug eruption (FDE) is a localized reaction to a systemic allergen that often involves the genitals. The tetracyclines are among the common causes, and owing to the frequent use of doxycycline and other tetracyclines in STD treatment and the high frequency of genital involvement, tetracycline-related FDEs are common in STD-related clinical practices. Other common causes of FDE include the sulfonamides, metronidazole, phenytoin, and phenolphthalein. The lesion typically resembles a burn, with initial pain and erythema and sometimes bulla formation, followed by superficial sloughing. Repeat FDE may recur in the same location as prior episodes. The reaction usually begins 7–10 days after initiating the offending drug, but with subsequent exposures the onset may be faster, sometimes within hours. Healing occurs without scarring, although hyperpigmentation may persist. Aside from discontinuing the offending drug, no specific treatment is available.
22–1. Fixed drug eruption of the penis. The patient had just finished a 7-day course of tetracycline HCl for NGU and complained of 3 days of pain “like a burn.”
22–2. Fixed drug eruption, with sharply demarcated erythematous lesions of the glans penis and finger web in a patient treated with doxycycline for chlamydial infection.
22–3. Fixed drug eruption presenting as a bulla of the glans penis
22–4. Fixed drug eruption of the penis.
Psoriasis
Psoriasis often involves the genitals and can mimic secondary syphilis, scabies, and keratoderma blennorrhagica of reactive arthritis. In addition to genital lesions, most patients with psoriasis have lesions of other commonly involved sites, such as the scalp and extensor surfaces of the elbows and knees, or pitted fingernails or toenails. All these areas should be carefully inspected. However, genital lesions may be the first or only manifestation. Sometimes biopsy is necessary for diagnosis.
22–5. Psoriasis of the penis. Having begun a new sexual relationship 2 weeks previously, the patient suspected STD; he also had a previously unrecognized patch of typical psoriasis of the scalp.
22–6. Psoriasis of the penis.
22–7. Psoriasis, with several psoriatic plaques (black arrows) in a woman with recurrent genital herpes (white arrow)
22–8. Penile hemorrhage due to corpus cavernosum fracture. The patient presented to an
STD clinic immediately following acute pain and swelling that began after his partner rolled
onto his erect penis.
STD clinic immediately following acute pain and swelling that began after his partner rolled
onto his erect penis.
Penile Fracture
Penile fracture is rupture of a corpus cavernosum, a rare event caused by forcible flexion of the penis
when erect. Surgery often is required to repair the capsule of the ruptured corpus in order to preserve
erection without deformation.
22–9. Sclerosing lymphangitis of the penis (arrow).
Penile Sclerosing Lymphangitis
Sclerosing lymphangitis of the penis sometimes follows vigorous sexual activity and presents as a firm, mobile, painless, elongated, subcutaneous mass typically in the coronal sulcus. Some cases may be slightly painful. No specific treatment is required; the mass typically resolves spontaneously over several weeks. Anecdotal reports suggest the condition is commonly associated with STDs, and up to 25% of patients are said to have gonorrhea, chlamydia, NGU, herpes or other STDs. Although this may be an artifact of STD clinic attendance by young men with genital lesions, it is reasonable to screen young men (age 20–40 years) with the syndrome for common STDs

22–10. Anal fissure in a man presenting with anal pain and occasional bleeding for
1 week.
1 week.
Anal Fissure
Anal fissures are common in all populations and probably are the most frequent cause of ulcerative lesions of the anus. Fissures may be initiated by trauma and probably are particularly frequent in men or women who participate in receptive anal intercourse. Anal fissures may be indistinguishable from syphilitic chancres and herpes. Sexually active persons who present with anal fissures should be asked about receptive anal sex and, if exposed, evaluated for STD.

22–11. Chronic rectal fistula with secondary gonococcal infection of the fistula tract.
Perianal Fistula
One year prior to presentation, this woman had a “boil” near her anus that drained spontaneously. Subsequently, there was a persistent “bump” that periodically drained small amounts of fluid and perhaps feces. She presented to an STD clinic with 1 week of pain and increased drainage from the lesion. A rectal fistula was diagnosed; Neisseria gonorrhoeae was isolated from her cervix, anal canal, and the fistula tract.

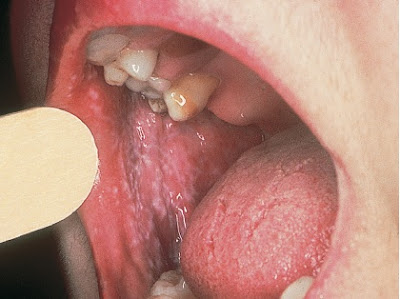
22–12. Genital ulcer due to Behçet syndrome in a 23-year-old woman born in Turkey, who presented
to an STD clinic fearing genital herpes. She also reported several years of severe recurrent oral
aphthous ulcers.
to an STD clinic fearing genital herpes. She also reported several years of severe recurrent oral
aphthous ulcers.
Behçet Syndrome
Behçet syndrome is a rare condition of probable autoimmune origin, occurring most frequently in persons of Mediterranean ancestry. It is manifested by recurrent oral and genital ulcers which may be deeply erosive, and often by conjunctivitis or uveitis. Complications include arthritis, erythema nodosum, cranial neuropathies, cranial arteritis, meningoencephalitis, stroke, blindness from retinal infarction, and psychosis. Treatment options include colchicine, corticosteroids, chlorambucil, other cytotoxic drugs, and biological antitumor necrosis factor-alpha drugs such as infliximab or etanercept.

22–13. Methicillin-resistant Staphylococcus aureus folliculitis of the pubic area and upper penile shaft. Pustular lesions and ulcers are limited to hair-bearing areas.

22–14. Bacterial folliculitis, showing hairs emerging from pustules (arrow).
Folliculitis
Folliculitis, by definition, originates in hair follicles. Bacterial folliculitis is often staphylococcal or streptococcal and can present in the pubic area, groin, buttocks, and perineum. Anecdotal experience in STD clinics suggest that the frequency of folliculitis may be rising in sexually active persons who shave the genital area, and some patients present with fear of herpes or other STD. The diagnostic hallmark of folliculitis is observation of a single hair emerging from some pustular lesions, helping distinguish the condition from herpes. In addition, folliculitis lesions generally are more widespread than those of genital herpes, and initial herpes generally involves the genitals per se rather than the pubic area, groin, or other hair-bearing areas.

22–15. Pyoderma of the penis in a patient with scabies; Staphylococcus aureus was isolated.

22–16. Penile pyoderma with necrotizing cellulitis in a man with secondary syphilis; Staphylococcus aureus and β- hemolytic Streptococcus pyogenes were isolated. This is the same patient whose secondary syphilis rash is shown; he gave a history of a painless ulcer at the corona of the penis for 6 weeks before onset of penile pain and swelling.
Genital Pyoderma
Pyoderma and cellulitis of the genitals usually result from secondary infection of preexisting lesions. Scabies is a common predisposing factor among patients in STD clinics. Secondary bacterial infection of herpetic lesions or syphilitic chancres appears to be uncommon, although a chancre probably was the initial lesion in the patient in Fig. 22–16. Parenteral antibiotic therapy may be required for severe cases.

22–17. Erythrasma.
Erythrasma
Erythrasma is a superficial cutaneous infection, typically of the genitals, upper thighs, and crural folds, caused by Corynebacterium minutissimum. Most cases are less extensive than illustrated in Fig. 22–17. Chronic cases typically present with a copper-colored, red-brown rash with a raised border and fine scale. Bright coral-red fluorescence is seen under ultraviolet light (Wood’s lamp). Erythrasma can be confused with tinea cruris (see Figs. 22–18 and 22–19), an important distinction as the treatments are different. Erythrasma is treated with oral clarithromycin or erythromycin; azithromycin probably would be effective but has not been studied.
Tinea Cruris
Tinea cruris is most common in men (“jock itch,” Fig. 22–18) but is not rare in women (Fig. 22–19). It is caused by dermatophyte fungi, including Trichophyton, Epidermophyton, and Microsporum species. Tinea pedis (athlete’s foot), caused by the same organisms, often is present simultaneously. Tinea cruris is characterized by an erythematous, papular, sometimes erosive dermatitis of the crural folds, inner thighs, or scrotum, with accentuated erythema and fine scale at the sharply demarcated border. The penis and labia usually are not involved. Tinea cruris can be confused with erythrasma (see Fig. 22–17) and other perigenital dermatoses, and the diagnosis can be difficult in dark-skinned patients, in whom erythema may be difficult to discern. Clinical diagnosis usually is reliable, but can be confirmed by scraping the advancing border and examining microscopically for fungal elements after digestion with 10% KOH. Topical imidazole creams such as miconazole (Micatin), ketoconazole (Nizoral), and others, as well as tolnaftate (Tinactin) and terbinafine (Lamisil) are effective; over-the-counter versions are readily available.

22–18. Tinea cruris, with annular scaling at the leading edge of the inflammatory
lesion extending from the inguinal fold to the thighs.

22–19. Tinea cruris.

22–20. Vitiligo of the penis.
Vitiligo
Vitiligo is acquired cutaneous depigmentation resulting from loss of melanocytes, of probable autoimmune pathogenesis. Any area of the skin may be involved, but patients with genital involvement may present with concerns about STD. Although functionally harmless, vitiligo can be psychologically debilitating when it involves cosmetically sensitive areas, including the genitals. Some patients respond to treatment with topical or systemic corticosteroids, phototherapy, topical immunomodulators, or surgically using punch grafting of normally pigmented skin. Proper management requires dermatological expertise.

22–21. Lichen simplex chronicus of the vulva, with an ulcer caused by excoriation.
Lichen Simplex Chronicus
Lichen simplex chronicus usually presents as a solitary plaque, often quite large, with thickening of the skin and accentuated markings (lichenification), erythema, and sometimes excoriation. Involvement of the scrotum and labia majora is typical. The condition is more common in women than men and often accompanies other pruritic dermatoses, especially atopic dermatitis. The clinical manifestations primarily result from habitual scratching, which may be unconscious, and lesions are most common on the side of the dominant hand. Topical steroids and instruction to avoid scratching often are effective and dressings may help prevent unconscious scratching during sleep.

22–22. Contact dermatitis of the penis in a patient who was allergic to the adhesive tape of a bandage used to cover an episode of recurrent genital herpes; healing herpetic lesions are visible between the patches of acute dermatitis.
Contact Dermatitis
In its fully developed form, allergic contact dermatitis is characterized by vesicles or a denuded, weeping skin surface. History of exposure to potential irritants or allergens often is present. Removal of the inciting agent usually results in prompt resolution, although topical steroids may speed improvement.
Lichen Planus
Lichen planus is one of the most common genital dermatoses and is seen frequently in patients at risk
for STD. The cause is unknown. The condition typically causes flat-topped papules with shiny surfaces, typically with a violaceous hue. Most lesions itch, but some are nonpruritic. Lichen nitidus (see Fig. 22– 26) is a variation of lichen planus that presents with multiple small papules. Oral or genital mucosal lesions often are present, with lacy, serpiginous striae. When the lateral aspect of the tongue is involved, lichen planus can mimic HIV-related oral hairy leukoplakia. Most cases respond to topical corticosteroids.
22–23. Lichen planus of the penis.

22–24. Lichen planus of the vaginal introitus,
with faintly violaceous, serpiginous striations.
Secondary lichenification of the labia minora
also is present
22–25. Lichen planus of the oral mucosa

22–26. Lichen nitidus, generally considered a micropapular variant of lichen planus.
A plaque of typical lichen planus is seen immediately proximal to the glans.

22–27. Fordyce spots of the penis.
Fordyce Spots
Fordyce spots are prominent but anatomically normal sebaceous glands, most commonly observed in women on the inner aspect of the labia majora, but other sites, including the penis, can be involved. Individual papules typically are white or yellow and may appear more prominent in the presence of surrounding erythema due to other inflammatory conditions. For example, some women first notice Fordyce spots in the presence of vulvovaginal candidiasis. Anxious patients who first notice Fordyce spots may be concerned about STD. No treatment is required.
Pearly Penile Papules and Tyson Glands
Pearly penile papules are normal anatomic variants that appear as small (usually 0.5–1 mm) shiny papules of the penile corona, sometimes with filiform morphology. They are present in 10–20% of men, regardless of race or skin color, and are more common in circumcised than uncircumcised men.
“Tyson gland” has been used in reference to various normal anatomic variants of the penis. As usually used, Tyson glands—also known as preputial glands—are prominent, specialized sebaceous glands of the penile corona and inner surface of the foreskin. Sometimes they present as pairs located symmetrically on the ventral aspect of the penis immediately proximal to the glans; one, two, or sometimes three pairs may be present. Some affected men become concerned about STD when they first notice pearly penile papules or Tyson glands, or when they observe other men without them, and inexperienced clinicians may confuse them with genital warts, molluscum contagiosum, or other lesions.

22–28. Pearly penile papules and Tyson glands. There are numerous pearly penile
papules along the corona of the glans penis; the larger white papules on the ventral
surface below the glans are Tyson glands.

22–29. Four Tyson glands, two on each side of the meatus; one gland is denoted by the white arrow.
Vestibular Papillomatosis
Vestibular papillomatosis is considered the female counterpart of pearly penile papules and typically presents with multiple soft papules of the vaginal introitus or labia minora, usually symmetrically distributed. The condition may be confused with genital warts by both patients and providers. As for pearly penile papules, Tyson glands, and Fordyce spots, vestibular papillomatosis is a normal anatomic variant.

22–30. Vestibular papillomatosis (black arrow); compare with genital warts (see Figs. 8–1 and 8–4) and pearly penile papules of the penis (see Fig. 22–28). The patient complained of vulvar pruritus and has a lesion consistent with recurrent genital herpes (white arrow).
REFERENCES
H. Hunter Handsfield, MD, Color Atlas & Synopsis of Sexually Transmitted Diseases, Third Edition.





















COMMENTS