These are the images, diagnosis and treatment of cases the disease caused by Pediculosis Pubis. This is a Scabies Disease
Scabies is cutaneous infestation with the itch mite, Sarcoptes scabiei. The organism is highly infectious and transmitted by close personal contact. Sexual exposure is a frequent mode of transmission, but infestation also is commonly acquired through shared bedding and clothing and sometimes nosocomially, especially in skilled nursing facilities and other chronic care settings. Scabies is among the most common dermatoses observed in persons attending STD clinics. The primary clinical manifestation is an intensely pruritic papular eruption, often with secondary excoriations; hyperkeratotic, nodular, vesicular, or bullous lesions sometimes occur. Most clinical manifestations result from hypersensitivity to the mite and its feces and ova, so that symptoms typically develop 2–4 weeks after acquisition of the first infestation but often within 1–2 days in subsequent infestations. In addition, hypersensitivity may result in persisting symptoms for a few weeks following successful scabicidal treatment. Secondary staphylococcal or streptococcal infection is common. An infrequent but important complication is crusted (“Norwegian”) scabies, characterized by extensive hyperkeratosis and large numbers of mites, sometimes seen in AIDS patients or persons taking high doses of corticosteroids.
EPIDEMIOLOGY
Incidence and Prevalence
• No accurate incidence data
• Epidemics tend to recur in 10–30 years cycles
• Diagnosed in up to 5% of STD clinic patients
Transmission
• Skin-to-skin contact or exposure to infested fomites, e.g., bed linens or shared clothing
• Sexual exposure may be the most common mode of acquisition in young adults
• Nonsexual contact accounts for many cases in households and other settings (e.g., hospitals, nursing homes, shelters)
Age
• All ages affected
Sex
• No special predilection
Sexual Orientation
• No special predilection
Other Risk Factors
• Settings of poor hygiene and crowding, e.g., homeless shelters
• Nosocomial transmission to health care workers sometimes occurs, especially if initial case has especially high organism load, as in crusted scabies
HISTORY
Incubation Period
• Typically 2–4 weeks from infestation to first symptoms for first episode
• Often as brief as 1–2 days for subsequent infestations, due to hypersensitivity
Symptoms
• Localized or generalized skin rash with intense itching, often worse at night or exacerbated by bathing
• Pruritus sometimes occurs on apparently uninvolved skin surfaces
• Absence of itching is evidence against scabies
Epidemiologic History
• Behavioral risks for STD
• History of exposure to scabies
• Communal living, especially in settings of poor hygiene
PHYSICAL EXAMINATION
• Papular skin rash, usually with secondary excoriations
• Most commonly involved sites are flexor surfaces of elbows, axillae, hands, finger webs, waist, ankles, dorsal surfaces of feet, genitals, buttocks, inguinal and gluteal folds
• Genital lesions often seen in patients seeking care in STD clinics
• Often 0.5–1.0-cm linear lesions that mark the paths of burrowing mites, sometimes with a leading black dot or small vesicle that marks the mite’s location
• Occasional vesicular, nodular, scaling, bullous lesions or eczematous plaques
• Secondarily infected pustules or localized cellulitis are common
• Crusted (Norwegian) scabies manifested by marked hyperkeratosis, fissures, and secondary infection
LABORATORY DIAGNOSIS
• Microscopy of scrapings of lesions, obtained with a scalpel blade and mixed with 10% KOH solution or mineral oil, showing mites, ova, or scybala (fecal pellets)
• Microscopy is insensitive; multiple scrapings often are necessary for diagnosis
• Biopsy occasionally required
DIAGNOSTIC CRITERIA
• Diagnosis usually is suspected on the basis of symptoms and clinical appearance
• Application of water-based ink followed by wiping with alcohol may highlight mites’ intracutaneous burrows (“burrow ink test”)
• Microscopic confirmation is recommended, especially for atypical cases
• Assessment of response to treatment (therapeutic trial) sometimes is helpful, but clinical response may be slow
TREATMENT
Regimens of Choice
• Permethrin 5% cream, applied to entire skin surface from neck down, washed off after 8–14 hours
• Ivermectin 250 μg per kg body weight PO, repeated in 2 weeks; regimen of choice for crusted scabies
• Symptomatic improvement may be delayed >2 weeks after successful scabicidal treatment, due to
hypersensitivity to slowly resorbed mites, ova, and scybala
Alternative Regimen
• Lindane 1% lotion (1 oz) or cream (30 g) applied to entire skin surface below the neck, washed off after 8 hours; because of risk of toxicity, should be used only if regimens of choice are unavailable or
ineffective
Ancillary Measures
• Launder or dry-clean bed linens and all clothing used within 48 hours prior to treatment
• Antihistamines (e.g., diphenhydramine, hydrazine) or other antipruritus drugs may speed symptomatic relief
• Antibiotics may be indicated if secondary bacterial infection is present
PREVENTION
• Mainstays are avoidance of high-risk sexual exposures, shared living quarters in settings of poor hygiene, and direct personal contact with infested persons
• Routinely treat sex partners and persons sharing living quarters with infested persons
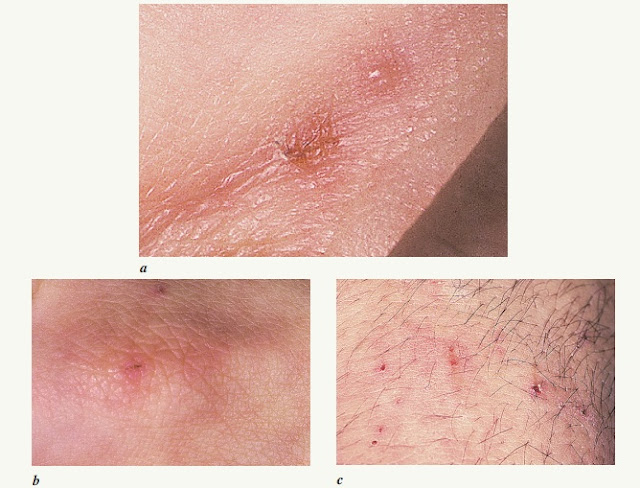
14–1. Scabies. a. Papules of finger web; one lesion has been excoriated. b. Papules of knuckle; note
dark line across papule, which yielded diagnostic scrapings. c. Excoriations on extensor surface of elbow
dark line across papule, which yielded diagnostic scrapings. c. Excoriations on extensor surface of elbow
CASE 1
Patient Profile Age 19, male carpenter
History Intense “itching all over” for 2 weeks, worse at night; onset 4 weeks after intercourse with an
unknown female partner
Examination Erythematous papules and excoriations of hands, elbows, around waist; genital examination normal
Differential Diagnosis Scabies, eczema, dermatitis herpetiformis, contact dermatitis
Laboratory Microscopic examination of lesion scrapings demonstrated ova and feces of S. scabiei;
screening urine NAAT) for Chlamydia trachomatis and Neisseria gonorrhoeae, VDRL, HIV serology; positive for C. trachomatis
Diagnosis Scabies; urethral chlamydia (asymptomatic)
Treatment Permethrin 5% cream; counseled to launder bed linens and clothing used in preceding
48 hours; azithromycin 1.0 g PO, single dose
Comment Symptoms and rash subsided gradually over 10 days; incidental chlamydial infection
illustrates importance of scabies as STD risk
14–2. Scabies of glans penis. Note similarity to secondary syphilis (see Fig. 5–14).
psoriasis (see Figs. 22–5 and 22–6), and keratoderma blennorrhagica of reactive arthritis
psoriasis (see Figs. 22–5 and 22–6), and keratoderma blennorrhagica of reactive arthritis
CASE 2
Patient Profile Age 37, homeless man living in a communal shelter
History Pruritic rash for 2 weeks, worse at night; no recent sexual exposure; scabies or itching reported to be common among other shelter residents
Examination Exfoliating papules on glans and shaft of penis; numerous papules, nodules, excoriations of trunk and extremities
Differential Diagnosis Scabies, secondary syphilis, keratoderma blennorrhagica (reactive arthritis),
psoriasis
Laboratory Scrapings negative for scabies; VDRL, HIV serology, urine NAAT for N. gonorrhoeae and C. trachomatis (all negative)
Diagnosis Scabies
Treatment Permethrin 5% cream
Comment The penis is a common site of scabies lesions, perhaps especially among infested persons who seek care in STD clinical settings. Despite negative scrapings, the diagnosis of scabies was secure based on clinical presentation and epidemiologic history. The patient’s symptoms and rash resolved over 2 weeks; the therapeutic response helped confirm diagnosis. The local health department inspected the shelter, diagnosed five additional cases of scabies, and arranged for treatment of all residents and simultaneous laundry of all clothing and bed linens.
14–3. Scabies mimicking genital herpes. The patients presented with painful, pruritic lesions of the
penis, which he had excoriated by scratching. Herpes was suspected but diagnostic tests were negative, and scabies was diagnosed by microscopy of scrapings of
similar lesions on the elbows and hands.
 |
| Crusted (Norwegian) scabies in a man with AIDS |
14–5. S. scabiei with ova, scraped from a scabies skin lesion. (Reproduced with
permission from KK Holmes, et al, eds. Sexually Transmitted Diseases. 3rd ed.
REFERENCES
H. Hunter Handsfield, MD, Color Atlas & Synopsis of Sexually Transmitted Diseases, Third Edition.














COMMENTS